
Background
Since the first documented laparotomy in 18091Bellis S, Surgery For An Acute Abdomen – An Intriguing History Of The Laparotomy Procedure. Cambridge Medicine Journal, 1-3, 2018. DOI: 10.7244/cmj.2018.12.002
https://cambridgemedicine.org/doi/cmj.2018.12.002, general surgery has been challenged by its inability to reliably manage a basic but fundamental aspect of the procedure – closure of the abdominal wall. Failure of the closure due to sutures tearing through tissue leads to incisional hernia, which some authors describe as occurring in up to 35.6% of cases2Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A, et al. (2015) Systematic Review and Meta-Regression of Factors Affecting Midline Incisional Hernia Rates: Analysis of 14 618 Patients. PLoS ONE 10(9): e0138745. DOI: 10.1371/journal.pone.0138745
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4577082/. While seemingly a straightforward mechanical problem, the potential impact of a failed abdominal closure can be devastating, with lifelong debilitation, morbidity, and re-operation occurring in a large percentage of patients3Holihan J, et al., Adverse Events after Ventral Hernia Repair: The Vicious Cycle of Complications. J Am Coll Surg. 2015 Aug;221(2):478-85. DOI: 10.1016/j.jamcollsurg.2015.04.026
https://pubmed.ncbi.nlm.nih.gov/26206646/.
Demonstrating the enormity of the problem, ventral hernia repairs are estimated at 611,000 cases per year in the United States4Schlosser, K.A., Renshaw, S.M., Tamer, R.M. et al. Ventral hernia repair: an increasing burden affecting abdominal core health. Hernia 27, 415–421 (2023). DOI: 10.1007/s10029-022-02707-6
https://pubmed.ncbi.nlm.nih.gov/36571666/, of which approximately 2/3 are from failed prior closure5Chavan, Sushrut Subhash et al. A clinical study on ventral hernias in a tertiary care hospital. International Surgery Journal 4 (2017): 2600. DOI:10.18203/2349-2902.isj20173106
https://www.ijsurgery.com/index.php/isj/article/view/1615, representing one of the most common general surgery procedures performed. One quarter of the repair procedures fail yet again6van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012 Aug;204(2):144-50. DOI: 10.1016/j.amjsurg.2012.01.012
https://pubmed.ncbi.nlm.nih.gov/22579232/, initiating a spiral into recurrent surgery and disability of profound magnitude. The clinical need for progress is self-explanatory.
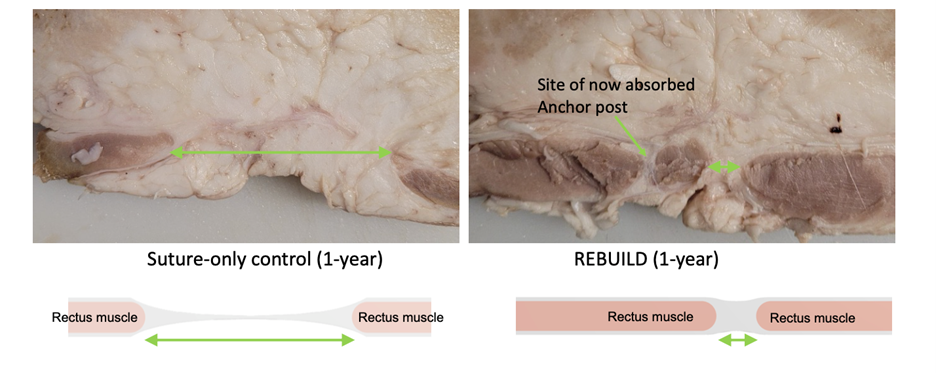
To that end, REBUILD Bioabsorbable (“REBUILD”) is an implantable, bioabsorbable anchor designed to support soft tissue approximation of the abdominal wall in conjunction with suture by distributing tension to maintain apposition of the rectus muscles during healing, which has been associated with reduction in post-operative ventral hernia formation.
The sterile, single-use anchors are made of PLGA [poly (lactic-co-glycolic acid)], a co-polymer used in numerous therapeutic devices with well-known biodegradability and biocompatibility properties. Each anchor is comprised of an Anterior and Posterior Component. A series of REBUILD anchors are placed on opposite sides along the length of the abdominal incision using instruments provided, and the incision is then closed using sutures passed through the REBUILD anchor posts and a standard technique in the midline.
The anchor design and bioabsorbable material, as well as the deployment instruments, are designed to preclude many of the problems associated with augmented abdominal wall closure today (particularly with mesh), such as:
- Complications from long-term foreign bodies,
- Chronic pain due to entrapment of intercostal nerves,
- Infection and seroma from broad dissection,
- More complicated (than suture alone) re-entry into the abdomen either acutely or later, and
- Cumbersome requirements for deployment.
Additionally, mesh is often deployed under minimal or no tension and therefore is not distributing forces of the midline closure. In such cases, mesh merely serves as a prosthetic backup for a failed midline – which perhaps explains the long-term failures seen in mesh repairs.
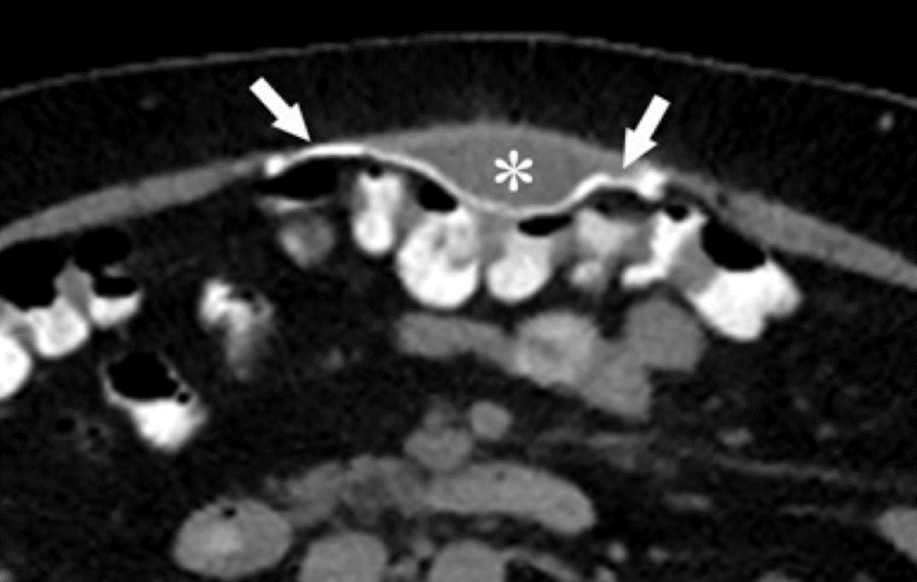
“Normal” journal7Gavlin, Alexander et al. Imaging and Treatment of Complications of Abdominal and Pelvic Mesh Repair. Radiographics : a review publication of the Radiological Society of North America, Inc vol. 40,2 (2020): 432-453. DOI:10.1148/rg.2020190106
https://pubs.rsna.org/doi/10.1148/rg.2020190106 result after mesh reconstruction. The * denotes a stable fluid collection between the mesh and the abdominal wall, but of note, the gap between rectus edges is several centimeters
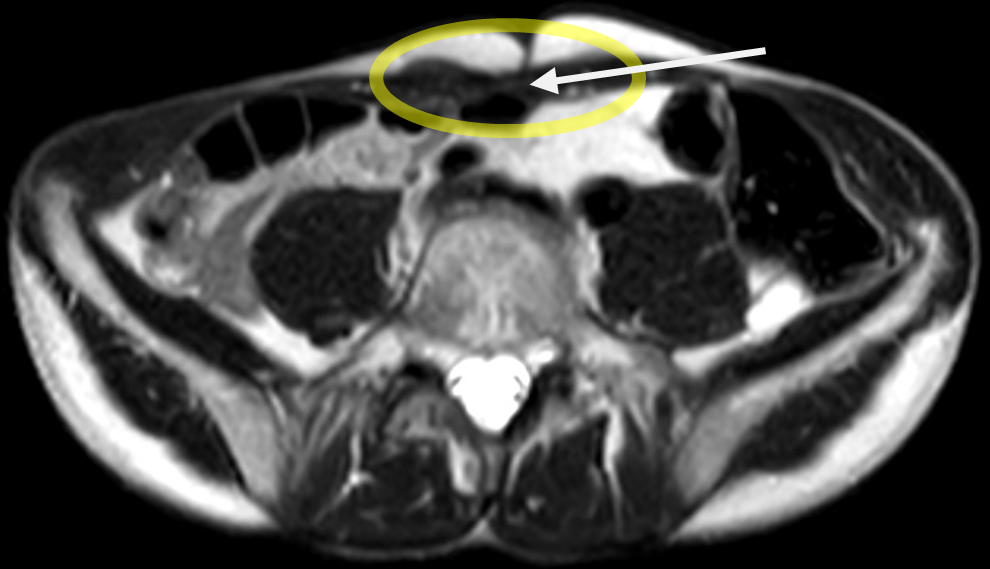
REBUILD study participant, demonstrating no gap (white arrow) between the opposing rectus abdominus muscles at 12-months
REBUILD is designed to specifically offload tension on the midline closure beginning at time zero. This supports apposition of the medial rectus muscle borders and promotes intrinsic linea alba (midline) healing. No other device is designed to perform in such a manner.
Furthermore, REBUILD is intentionally designed not to impact abdominal wall function, either from permanent foreign material or broad dissection and/or intercalation required for deployment. For example, REBUILD:
- Is absorbed within approximately 1 year (with individual variation), thus eliminating the risk of long-term foreign body complications.
- Is placed well-medial of intercostal nerve trunks, thus addressing the risk of nerve entrapment and associated chronic pain.
- Requires no broad dissection (dead space creation) either within or anterior to the abdominal wall.
- Requires no special maneuvers to re-enter the abdomen for post-operative emergencies or disease recurrences. As an example, one of the participants in a REBUILD clinical trial required urgent re-entry for hemorrhage. The surgeon was able to cut the sutures, access the abdomen, and then reuse the same (already deployed) anchors for closure (of note, a similar but analogous earlier version of REBUILD).
- 1Bellis S, Surgery For An Acute Abdomen – An Intriguing History Of The Laparotomy Procedure. Cambridge Medicine Journal, 1-3, 2018. DOI: 10.7244/cmj.2018.12.002
https://cambridgemedicine.org/doi/cmj.2018.12.002 - 2Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A, et al. (2015) Systematic Review and Meta-Regression of Factors Affecting Midline Incisional Hernia Rates: Analysis of 14 618 Patients. PLoS ONE 10(9): e0138745. DOI: 10.1371/journal.pone.0138745
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4577082/ - 3Holihan J, et al., Adverse Events after Ventral Hernia Repair: The Vicious Cycle of Complications. J Am Coll Surg. 2015 Aug;221(2):478-85. DOI: 10.1016/j.jamcollsurg.2015.04.026
https://pubmed.ncbi.nlm.nih.gov/26206646/ - 4Schlosser, K.A., Renshaw, S.M., Tamer, R.M. et al. Ventral hernia repair: an increasing burden affecting abdominal core health. Hernia 27, 415–421 (2023). DOI: 10.1007/s10029-022-02707-6
https://pubmed.ncbi.nlm.nih.gov/36571666/ - 5Chavan, Sushrut Subhash et al. A clinical study on ventral hernias in a tertiary care hospital. International Surgery Journal 4 (2017): 2600. DOI:10.18203/2349-2902.isj20173106
https://www.ijsurgery.com/index.php/isj/article/view/1615 - 6van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012 Aug;204(2):144-50. DOI: 10.1016/j.amjsurg.2012.01.012
https://pubmed.ncbi.nlm.nih.gov/22579232/ - 7Gavlin, Alexander et al. Imaging and Treatment of Complications of Abdominal and Pelvic Mesh Repair. Radiographics : a review publication of the Radiological Society of North America, Inc vol. 40,2 (2020): 432-453. DOI:10.1148/rg.2020190106
https://pubs.rsna.org/doi/10.1148/rg.2020190106